Terms & Condition
We recommend you to kindly read the Terms of Use (hereinafter referred to as "Agreement") and the linked Privacy Policy, Disclaimer (as posted elsewhere on the Website) carefully before using the website www.mcxtra.com ("Website") or its mobile app ("Application") or both. This agreement sets forth the legally binding terms and conditions for your use of the Website and/or Application. By using the Website and/or Application and the services provided via the Website and/or Application ("Services"), you confirm that you have read, understood and agree to these Terms of Service.
If you do not agree to these Agreement, you must cease use of the Services and Website immediately.
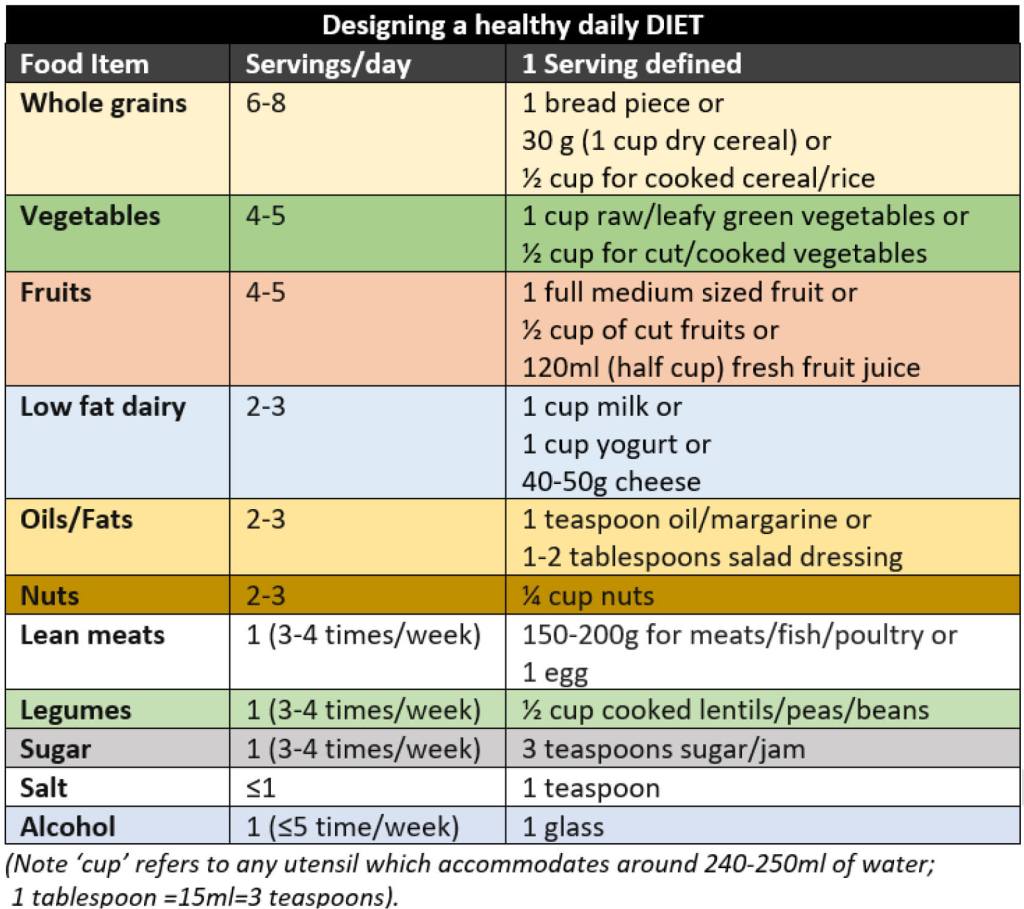
Reach Ajcon Technologies Private Ltd (hereinafter referred to as "RATPL") is a technology provider and facilitator that operates the Website http://www.mcxtra.com and its mobile app as a platform to provide users to upload their existing as well as new insurance policies (including Life, Health, Motor, Travel & Home Insurance policies) electronically which they may have bought from any insurer through any intermediary or directly at any point in time. The Website and the Application also provide the option to the users to seek assistance at any point in time pertaining to the policies that have been uploaded by them. This service can be availed through phone call, chat option, e-mail and scheduling a video conference with one of our experts. Users can also locate a garage or hospital in and around a pre- defined radius from the current location. Certain services/functions provided by RATPL can only be used once our Application is downloaded.
The user (hereinafter referred to as "you", or "your") will be subject to the rules, guidelines, policies, terms and conditions applicable to any Service that is provided by this Website/Application, and they shall be deemed to be incorporated into and form an integral part of this Agreement.
MEMBERSHIP ELIGIBILITY
Services are available only to, and may only be used by, individuals who are 18 years and above, who can form legally binding contracts under applicable law. You represent and warrant that you are at least 18 years old and that all registration information you submit is accurate and truthful. RATPL & may, at their sole discretion, refuse to offer access to or use of the Website or Application to any person or entity and change its eligibility criteria at any time. This provision is void where prohibited by law and the right to access the websites is revoked in such jurisdictions.
Individuals under the age of 18 may use services provided by RATPL & through its Website/Application however they must at all times do so only in conjunction with and under the supervision of a parent or legal guardian who is at least 18 years of age. In all cases, the adult is the user and is responsible for any and all activities done by the Individuals under 18 years of age.
INTRODUCTION
Using the Website www.mcxtra.com or its Application in any manner, including but not limited to visiting or browsing the Website, constitutes acceptance of this Agreement, including those additional terms and conditions and policies referenced herein and/or available by hyperlink. This Agreement applies to all the users of this Website and/or Application, including without limitation, users who are vendors, customers, merchants, contributors of content, information and other materials or services on the Website. If this Agreement conflicts with any other documents, the Agreement will control for the purposes of usage of the Website. If you do not agree to be bound by this Agreement and the Privacy Policy, you may refrain from using the Website and/or Application in any manner. RATPL reserves the right, to change or otherwise modify the Agreement without any prior notice, any time at its sole discretion. Your continued access or use of this Website would mean your acceptance of the updated or modified Agreement.
You hereby authorize RATPL & to access your insurance policies saved and stored in Policy Vault, personal data or information as defined herein below, for sending you renewal notices / reminders through e mail, sms or through phone calls, voluntarily calling you and giving you appropriate advise pertaining to any of your existing/ lapsed policies saved in Policy Vault or providing you feedback on the clarifications or assistance sought by you if any, assisting you in resolution of service issues pertaining to the insurance policies saved in Policy Vault, irrespective of the insurer or the intermediary that you have bought the policy from or through.
Personal data or information would mean you and your family member's details and include but not limited to E Mail id, Date of Birth, Mobile number, Name and Relationship, Blood Group, Allergies, details of existing or lapsed insurance policies etc.
YOUR REGISTRATION
You can register on the Website/Application through [Register now] option available on the Website/Application or through third party applications (including Facebook, Google+ etc.). Upon successful registration to the Services and payment of the annual subscription fee, unless waived, your policy vault would be activated within 72 hours of your uploading the insurance policy/ policies. In cases of active policy vaults, any new insurance policy that is uploaded would be decoded after 72 hours and would reflect in your vault once it has been decoded. You agree and understand that you are solely responsible for maintaining the confidentiality of your password which, together with your login ID, allows you to access the Service. That Login ID and password, together with any mobile number or other contact information you provide, forms your "Registration Information".
By providing us with your email address and mobile number, you agree to receive all required notices and information electronically, to that email address or mobile number. It is your responsibility to update any changes to your email address and mobile number. If you become aware of any unauthorized use of your Registration Information, you agree to notify RATPL immediately. RATPL & shall not be liable for any unauthorized use or access. You expressly agree and acknowledge that in case of any breach of your User Login and Registration details due to any data hack, malware attack or breach, RATPL shall not be responsible and liable.
Policy Vault and Assist Me services are only applicable to insurance policies whether purchased in India or abroad, but through an insurance company registered with Insurance Regulatory and Development Authority of India ("IRDAI") in India.
ACCURATE REGISTRATION INFORMATION
You shall provide true, accurate, current and complete information about yourself and undertake to inform/update of any change in your Registration Information promptly and keep it up-to-date and accurate at all times, as it has a direct bearing on the provision of Services by RATPL and its affiliates. You agree not to misrepresent your identity nor will you make an attempt to make an unlawful access to the Website and/or Application or use of the Services.
Policy Vault also allows you to save insurance policies of your family members including your spouse, dependent children, parents and parents in law, who might have authorized you in this regard, in which case you shall be acting under proper authorization from your family members. By uploading policies of such family members, you represent and confirm that you are duly authorized by them in this regard and shall absolve RATPL from any and all claims arising out of any claim for breach of privacy, unlawful access etc. by your family members/entity. RATPL shall not be responsible for any such claims raised by any third party including your family members.
Any misrepresentation in providing the Registration Information shall render the Services void ab initio, but without any recourse on RATPL or its affiliates. RATPL shall not be held responsible for any reason whatsoever if the Registration Information is incorrect at any point in time. Failure to provide accurate and complete information during registration may prohibit the use of some services provided by RATPL & .
PROHIBITED , QUESTIONABLE AND INFRINGING ITEMS AND ACTIVITIES
The user is solely responsible for the conduct and activities on and regarding to Website and/or Application and any and all data, text, information, usernames, graphics, images, photographs, profiles, audio, video, items, and links (together, "Content") that you submit, post, and display on the Website.
Your Content and your use of Website and/or Application shall not:
- Be false, inaccurate or misleading.
- Infringe upon any third-party's copyright, patent, trademark, trade secret or other proprietary or intellectual property rights or rights of publicity or privacy.
- Violate this Agreement or any applicable law, statute, ordinance or regulation.
- Be defamatory, unlawfully threatening, unlawfully harassing, impersonate or intimidate any person (including staff of RATPL / its affiliates or other users), or falsely state or otherwise misrepresent your affiliation with any person, through for example, the use of similar email address, nicknames, or creation of false account(s) or any other method or device
- Be obscene, illegal content or contain child pornography.
- Contain or transmit any code of a destructive nature that may damage, detrimentally interfere with, surreptitiously intercept or expropriate any system, data or personal information.
- Take any actions that may undermine or discredit the www.mcxtra.com feedback and ratings systems.
- Attempt to decompile, reverse engineer, disassemble or hack the Services or Sites (or any portion thereof), or to defeat or overcome any encryption technology or security measures implemented by www.mcxtra.com with respect to the Services and/or data transmitted, processed or stored by www.mcxtra.com
- Harvest or collect any information about or regarding other www.mcxtra.com account holders, whether through automated means, such as harvesting bots, spiders, robots or scrapers ("Automated Data Collection"), or otherwise, including, without limitation, any personal data or information.
- Upload, post, email, transmit or otherwise make available any unsolicited or unauthorized advertising, promotional materials, "junk mail", "spam", "chain letters", "pyramid schemes", or any other unauthorized form of solicitation.
- Modify, adapt or hack www.mcxtra.com or modify another website so as to falsely imply that it is associated with www.mcxtra.com
- Take any action or engage in any conduct that could directly or indirectly damage, disable, overburden, or impair the Services or the servers or networks connected to the Services.
- Appear to create liability for www.mcxtra.com or cause www.mcxtra.com to lose (in whole or in part) the services of www.mcxtra.com ISPs or other suppliers.
- Use the Services to violate the privacy of others or to "stalk" or otherwise harass others.
- Use the Services to collect, try to access or store personal data about other Users in connection with the prohibited conduct and activities set forth above.
- Link directly or indirectly, reference or contain descriptions of goods or services that are prohibited under this Agreement, the Privacy Policy, or other policy documents as posted on www.mcxtra.com.
CONTENT
You grant RATPL the non-exclusive, worldwide, perpetual, irrevocable, royalty-free and database rights to use any information or content you supply to RATPL & with, in any media now known or not currently known, with respect to your personal information or that of your family members or insurance policies that you upload on the Website. You agree to allow RATPL and its affiliate companies to pre-screen the data / insurance policies being uploaded by you and re-format your content if required, extract relevant information from the files you upload like renewal date etc., in order to fill the missing fields or make corrections wherever required in relevant sections of www.mcxtra.com Website and/or Application.
As part of a transaction, you may obtain personal information, including email address, mobile phone number, and address information, from another user of the Website and/or Application. Without obtaining prior permission from the other user, this personal information shall only be used for that transaction or for RATPL related communications. RATPL has not granted you the permission to use the information for unsolicited commercial messages, or to disseminate such information on any public platform, including its Website and/or Application. Without limiting the foregoing, without express consent from the user, you are not authorized to add any www.mcxtra.com user to your email or physical mail list. For more information, see our Privacy Policy.
RATPL considers any unsolicited suggestions, ideas, proposals or other material submitted to it by users via the Website and/or Application or otherwise (other than the insurance policies) to be non-confidential and non-proprietary, and RATPL shall not be liable for the disclosure or use of such material. If, any member sends material to improve the Website at the request of any director or employee of RATPL or its affiliates, RATPL will also consider that material to be non-confidential and non-proprietary and RATPL will not be liable for use or disclosure of the material. Any communication by you to RATPL through the Website and/or Application or otherwise is subject to this agreement. You hereby grant and agree to grant RATPL, under all of your rights in the Material, a worldwide, non-exclusive, perpetual, irrevocable, royalty-free, fully-paid, right to incorporate, use, publish and exploit such material for any purpose whatsoever, commercial or otherwise, including but not limited to incorporating it in the documentation, or any product or service, without compensation or accounting to you and without further recourse by you.
ACCESS TO PASSWORD / PROTECTED / SECURE AREAS
Access to and use of password protected and/or secure areas of the Website and/or Application is restricted to authorized users only. Unauthorized individuals attempting to access these areas may be subject to prosecution
MODIFICATION AND NOTIFICATION OF CHANGES
RATPL reserves the right to make changes to the Website and/or Application, related policies and agreements, this Agreement, the Privacy Policy and the Disclaimer at any time. If RATPL makes a material modification to this Agreement, it may notify you by: (i) displaying an announcement above the text of this Agreement or the Privacy Policy or any other place, as it deems appropriate, for thirty (30) days, being deemed sufficient notification, of such changes. After notice of a modification to the Agreement or the Privacy Policy has been posted for 30 days, the notice will be removed. If you have not used the Website for more than 30 days, you should check the User Agreement and/or Privacy Policy prior to any further use of the Website. Should you wish to terminate your account due to a modification to the User Agreement or the Privacy Policy, you may do so by sending an email to grievance@mcxtra.com with the subject line "Termination" to the following email address: If you choose to continue using the Services, you agree that by doing so you will be deemed to accept the new Agreement or Privacy Policy, as relevant.
LIMITATION OF WARRANTIES
By using our Website or Application or both, you understand and agree that all Services we provide are "as is" and "as available". This means that we do not represent or warrant to you that:
- The use of our Services will meet your needs or requirements.
- The use of our Services will be uninterrupted, timely, secure or free from errors.
- The information obtained by using our Services will be fully accurate or reliable, and
- Any defects in the operation or functionality of any Services we provide will be repaired or corrected.
Furthermore, you understand and agree that:
- Any content downloaded or otherwise obtained through the use of our Services is done at your own discretion and risk, and that you are solely responsible for any damage to your computer or other devices for any loss of data that may result from the download of such content.
- No information or advice, whether expressed, implied, oral or written, obtained by you from RATPL or through any Services, shall create any warranty, guarantee, or conditions of any kind, except for those expressly outlined in this Agreement.
- Some of the information displayed on the Website/Application is received from third parties such as details of curated insurance, contact details, Hospital and garage locators, cashless facilities, branch addresses of insurers etc. RATPL only displays such information on an as-is-where-is basis and does not independently verify such information. RATPL shall not, in anyway, be responsible or liable for correctness and accuracy of such information and the User itself should check veracity of such information.
LIMITATION OF LIABILITY
In conjunction with the Limitation of Warranties as explained above, you expressly understand and agree that any claim against RATPL and its affiliates, officers, employees, partners and licensors shall be limited to the amount you paid as service fees to Website and/or Application in connection with usage of this Website or Application or both, if any, for use of products and/or services.
You expressly understand and agree that RATPL and its affiliates, officers, employees, partners and licensors shall not be liable for any damages whatsoever, whether direct, indirect, incidental, consequential or exemplary including, but not limited to, damages for loss of data or other intangible losses, resulting from use of this Website, content, any related services, or as a result of any changes, data loss or corruption, cancellation, loss of access, or downtime to the full extent that applicable limitation of liability laws apply.
You acknowledge and agree that your only right with respect to any dissatisfaction with the services is to request for termination of your account and or discontinue any use of the services provided by the Website.
If, notwithstanding the previous sections, RATPL is found by a court of law to be liable in any manner, then, to the maximum extent permitted by law, RATPL's liability and that of its officers, directors, creators, employees and suppliers, to you or any third parties will be limited to a maximum amount of fee paid by the User to RATPL/ for the use of Services.
INFORMATION CONTROL
RATPL does not control the content provided by users that is made available on its Website and, as such, does not guarantee the accuracy, integrity or quality of such content. You may find some content to be offensive, harmful, inaccurate, or deceptive. There are also risks of dealing with underage persons or people acting under false pretense.
You acknowledge that RATPL may or may not pre-screen content, but that RATPL and its designees shall have the right (but not the obligation) in their sole discretion to pre-screen, refuse, delete or move any content:
- that violates these terms of use;
- if we receive a complaint from another User;
- if we receive a notice of intellectual property infringement or other legal instruction for removal; and/or
- if such Content is otherwise objectionable.
We may also block delivery of a communication (including, without limitation, feedback, postings, messages and/or chats) to or from the Services as part of our effort to protect the Services or our users, or otherwise enforce the provisions of this Agreement.
You acknowledge, and consent to and agree that RATPL and its affiliates may access, preserve and disclose your account information and content if required to do so by law or pursuant to an order of a court or by any governmental or regulatory authority having jurisdiction over RATPL or in a good faith belief that such access preservation or disclosure is reasonably necessary to:
(a) comply with legal process;
(b) enforce these terms of use;
(c) respond to claims that any content violates the rights of third parties; or
(d)protect the rights, property or personal safety of www.mcxtra.com, its users and/or the public.
SERVICES
RATPL is working with / in collaboration with third parties who specialize in providing respective services and have aggregated / created a network of hospitals - service centers
RATPL is working in collaboration with third parties to provide a network of third party repair and servicing workshops ("garages") for motor vehicles and providing road side assistance. RATPL is also working in collaboration with third parties to provide a network of hospitals and for providing health services and ambulance services in case of any emergency. It is clarified that RATPL is only acting as an aggregator and a facilitator for arranging these services relating to Garages and Hospitals and does not provide these services in any capacity whatsoever. The repair/servicing facility for any motor vehicle will be provided/done by the garage in their capacity as an independent service provider at vehicle owner's sole risk. These services are provided by the third parties on an 'as-is-where-is' basis and RATPL does not provide any warranties or makes any representations for these services. RATPL does not endorse the services of the garages / hospitals / road side assistance / ambulance services. RATPL and its affiliates shall not be liable for any payment obligation in relation to any kind of insurance claims and/or repairs /services, which shall be user's sole responsibility.
RATPL or its affiliates shall not be liable for any act(s)/omission(s) of the garages, hospitals and/or any defect/deficiency in repairs/services.
Any guarantee for timelines in relation to the services are subject to external factors and force majeure. RATPL and its affiliates shall not be liable for any time guarantee including for servicing, providing of any information as may be required or needed by the User instantly and/or delivery of vehicle, admission in hospital, providing of road side assistance or ambulance services when the Red Button is pressed due to any extraneous circumstances including any force majeure/act of god conditions.
Any third party facility/offer(s)/service(s)/product(s) shall be subject to the terms and conditions of such third party which shall be applicable to the user. RATPL does not endorse, makes no representation and shall have no liability or obligation whatsoever in relation to such third party facility/offer(s)/service(s)/product(s). All such third party facility/offer(s)/service(s)/product(s) shall be availed by user at their own risk. RATPL or its affiliates shall not be liable for any payment obligation in relation to such third party facility/offer(s)/service(s)/product(s), which shall be user's responsibility unless specifically agreed in writing.
RATPL reserves the sole right to modify, amend, change or revoke the claim services, any other services, any offers including third party facility/offer(s)/service(s)/product(s) herein at any time without assigning any reason and without any notice.
These terms and conditions for express claim services are in addition to all other terms and conditions provided here under and all these terms and conditions shall be applicable to you. RATPL reserves the right to sole right to modify, amend, change or revoke these terms and conditions without any notice.
Any disputes arising pursuant to these terms and conditions are subject to the exclusive jurisdiction of courts in Mumbai.
TERMINATION OF USAGE
You agree that RATPL, at its sole discretion, suspend or terminate your access to all or part of our Website and/or Application and resources with or without notice and for any reason, including, without limitation, breach of this user Agreement. Any suspected illegal, fraudulent or abusive activity may be grounds for terminating your relationship and may be referred to appropriate law enforcement authorities. Upon suspension or termination, your right to use the resources we provide will immediately cease, and we reserve the right to remove or delete any information that you may have on file with us, including any account or login information.
Notwithstanding any other provisions of this Agreement, or any general legal principles to the contrary, any provision of this Agreement that imposes or contemplates continuing obligations on a party will survive the expiration or termination of this Agreement.
PRIVACY
Your privacy is very important to us, which is why we've created a separate Privacy Policy in order to explain in detail how we collect, manage, process, secure, and store your personal information. Our privacy policy is included under the scope of this Agreement. Please click on privacy policy to read it in its entirety.
COPYRIGHTS / TRADEMARKS
All content and materials available on Website and/or Application, including but not limited to text, graphics, website name, code, images and logos are the intellectual property of RATPL, and are protected by applicable copyright and trademark law. Any inappropriate use, including but not limited to the reproduction, distribution, display or transmission of any content on this Website is strictly prohibited, unless specifically authorized by RATPL or any of its affiliate companies.
NON GUARANTEE
RATPL does not guarantee continuous, uninterrupted access to the Website and/or Application, and operation of the Website and/or Application may be interfered with by numerous factors outside RATPL's control. RATPL expressly disclaim all warranties and conditions of any kind, whether express or implied, including, but not limited to the implied warranties and conditions of merchantability, fitness for a particular purpose and non-infringement.
In addition, no advice or information whether oral or written obtained by you from Website and/or Application shall create any warranty. You acknowledge that the entire risk arising out of the use or performance of the Website and/or Application and /or the services remains with you to the maximum extent permitted by applicable law.
INDEMNITY
You agree to indemnify and hold RATPL and all its affiliates / subsidiaries (and its officers, directors, agents, subsidiaries, joint ventures, and employees) harmless from any and against any claims, causes of action, demands, recoveries, losses, damages, fines, penalties or other costs or expenses of any kind or nature, including reasonable attorneys' fees, or arising out of or related to your breach of this Agreement, your violation of any law or the rights of a third party, or your use of the Website/Application.
GOVERNING LAW
This Agreement shall in all respects be interpreted and construed with and by the laws of India since Website and/or Application is operated and controlled by RATPL.
Since the Website can be accessed by most countries around the world, few countries may have laws that differ from those in India. By accessing the Website and/or Application, you agree that the statutes and laws of Republic of India, will apply to all matters relating to the use of this Website and/or Application and the purchase of any products or services through this Website.
Furthermore, any action to enforce this User Agreement shall be brought in the courts located in Mumbai, India. You hereby agree to personal jurisdiction by such courts, and waive any jurisdictional, venue, or inconvenient forum objections to such courts.
DISCLAIMER
Though every possible effort has been taken to ensure that correct information is provided about product brochures, claim forms, policy wordings, claims settlement ratios, insurer offices, insurance quotient / quiz, ombudsman offices, list of hospitals and garages based on the information provided by the insurers or uploaded on their website / elsewhere in the public domain. It is made abundantly clear that Reach Ajcon Technologies Private Ltd ("RATPL") & its subsidiaries, directors, shareholders, officers, employees and www.mcxtra.com ("Website") are in no way responsible for any kind of error occurring or incorrect information being made available due to any changes made by the insurer or errors & omission by staff of RATPL and its subsidiaries.
Neither RATPL nor any of its subsidiaries is responsible for the accuracy or reliability of any data and/or information from any third party and does not guarantee continuous, uninterrupted access to the Website or availability of any services on its Website or its mobile application ("Application") made by RATPL on any kind of device, as a result of any action taken by RATPL or any third party. Operation of the Website and/or Application may be interfered with or by numerous factors beyond our control.
RATPL or any of its subsidiaries makes no representations, warranties or guarantees, express or implied regarding the accuracy, reliability or completeness of the content on its Website or Application or of the services provided by RATPL or any of its subsidiaries. It expressly disclaims any warranties or non-infringement or fitness for a particular purpose. RATPL makes no representation, warranty or guarantee that the content that may be available through the services is free of infection from any viruses or other code or computer programming routines that contain contaminating or destructive properties or that are intended to damage, surreptitiously intercept or expropriate any system, data or personal information.
RATPL, and its service providers make no warranty (i) that the services being offered through its Website and/or Application will meet your requirements, (ii) that the services will be uninterrupted, timely, secure, or error free, (iii) that the results that may be obtained from the use of such services will be accurate or reliable, (iv) that the quality of any products, services, information provided by our team related to your existing or new insurance policies will meet your expectations, (v) that the time taken to resolve your query or service your request or provide feedback to any clarification sought by you pertaining to your existing insurance policy or any new insurance policy, may exceed the given timelines for reasons beyond our control or on account of delay at the insurer's end (vi) that any errors in the technology will be corrected.
Any material downloaded or otherwise obtained through the use of the services of the Website and/or Application is done at your own discretion and risk and you will be solely responsible for any damage to your computer system or any other device or loss of data that results from the downloading of any such material.
RATPL reserves the right to modify or terminate the service for any reason, without notice, at any time. RATPL further reserves the right to alter the Terms of Use or other Site policies at any time. You are advised to review the policies frequently. If RATPL makes a material change in its policies or terms, it will notify you here, or by email, or by means of a notice on home page of the Website, or any other place RATPL deems appropriate. What constitutes a "material change" will be determined by RATPL's at its sole discretion, in good faith, and using common sense and reasonable judgment.
 Blog
Blog